-
Case Report :
Complex Venous and Arterial Reconstruction with Deep Vein After Pelvic Exenterative Surgery
AHSAN T. ALI, M.D./ G. PATRICK CLAGETT, M.D.,+ MICHAEL J. EDWARDS, M.D.*
From the *University of Arkansas for Medical Sciences, Little Rock, Arkansas; and the f University of Texas Southwestern at Dallas, Dallas, Texas
Effective local regional control for solid tumor malignancies is dependent upon prerequisite surgical excision with negative margins. Invasion of contiguous adjacent structures, particularly in anatomical spaces of limited size, may preclude the surgical goal of histologically negative margins. From a historical perspective, the invasion of vascular structures in the pelvis has proved to be a significant limitation in achieving local regional disease control with surgical resection.
In recent years, advances in the field of vascular surgery have caused us to reassess the his- torical criteria of resectability when blood vessels are focally invaded by malignancy. En bloc resection of adjacent vessels has been reported primarily with head and neck extirpations and increasingly with hepatobiliary and pancreatic lesions. In many cases, where the local vasculature is invaded or impinged by the tumor, venous structures are often ligated while arteries are bypassed wilh an appropriate conduit. In pelvic exenterative surgery, significant morbidity from chronic limb edema and deep venous thrombosis may result from the ligation of larger veins. This is especially the case when multiple major venous structures such as the common and the external iliac vein, as well as the hypogastric vein, are all simultaneously interrupted. To the best of our knowledge, there is no prior report examining venous reconstruction using the femoral vein for pelvic exenterative surgery requiring major iliac artery and venous resection. Herein we describe a case of a complex vascular reconstruction after pelvic exenterative surgery in a patient with recurrent rectal cancer invading multiple adjacent contiguous structures, including the iliac ves- sels.
A 70-YEAR-0LD MAN PRESENTED with left-sided flank pain and hydronephrosis of the left kidney. Past surgical history was significant for low anterior resection for rectal cancer 5 years ago. On computed tomography scan, he was found to have a 7 x 10 cm irregular mass in the left pelvis, which was suspicious for a recutrent rectal cancer. PET scan findings were consistent with a recurrent rectal cancer. Staging evaluation showed no metastatic foci for recurrent carcinoma. At surgery, he required an obturator and iliac lymph node dissection and an en bloc left colectomy, a left ureterectomy. and a partial cystectomy. Operative findings also revealed that the mass was adherent to the left common iliac vein and the common iliac artery at the bifurcation (Fig. 1).
Address correspondence and reprint requests to Ahsan T. Ali. M.D.. Assistant Professor of Surgery. University of Arkansas for Medical Sciences. 43 10 West Markham St.. #520. Little Rock. AR 72205.
In order to obtain negative margins, vascular resection and reconstruction were necessary. Proximal and distal contiol of the left common and external iliac veins was obtained. The left hypogastric vein and artery could not be conttolled initially due to the mass lying antetior to the hypogastric vessels. The common iliac vein and the external iliac veins were divided, which allowed for exposure to the bifurcation of the common iliac artery. Proximal and distal control was obtained tor the common iliac artery and the external iliac artery. The pelvic tiiass was resected en bloc. which included part ot the arterial wall ofthe common iliac and the external iliac artery at the bifurcation as well as the common iliac, hypogastric. and external iliac veins (Fig. 2). Once the mass was removed, the internal iliac artery and vein were suture ligated. On frozen section, margins were negative for malignancy. Reconstruction of the iliac artety was done with a vein patch restoring arterial inflow to the leg. The right (contralateral) superficial femoral veiti was harvested for a 12- to 14-cm length. End-to-end anastomosis was then performed using superficial femoral vein (SFV) as an interposition graft between the left common iliac
VENOUS AND ARTERIAL RECONSTRUCTION
Ali et ai
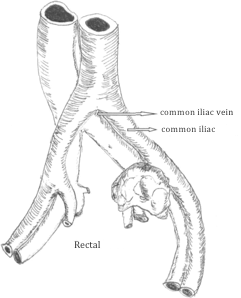
FIG. 1. Rectal lumor seen at the iliac vessels bifurcation.
vein and the left extemal iliac vein (Fig. 3). Valve in the eonduit was preserved. Extra caution was exerci. sed to prevent an air embolism by flushing the anastomosis under water before unclamping. Heparin was reversed after the reconstruction was completed.
Discussion
Radical tumor resection in the retroperitoniuni and the pelvis can result in significant morbidity.1 Tumor resectability is dependent on the extent of local invasion of contiguous structures, particularly the adjacent vasculature. Reconstruction of large central vessels was first described using a homograft one-half century ago by Crawford and Debakey.2 Unlike arterial reconstruction, venous bypasses are prone to postoperative thrombosis. Although ligation is always an option, it can result in massive limb swelling when all three ipsilateral major veins are acutely interrupted.1 The problem can be compounded in a patient with previous pelvic radiation and/or surgery where the lymphatics are compromised. Simultaneous arterial and venous reconstruction in retroperitonium or pelvis using a.synthetic graft has been described by Piquet et al3

FIG. 2. En-bloc resection of the tumor with the left coninion iliac, external iliac, and internal iliac veins. Removal of the arterial wail at the biftircation. Internal iliac artery and vein ligated.
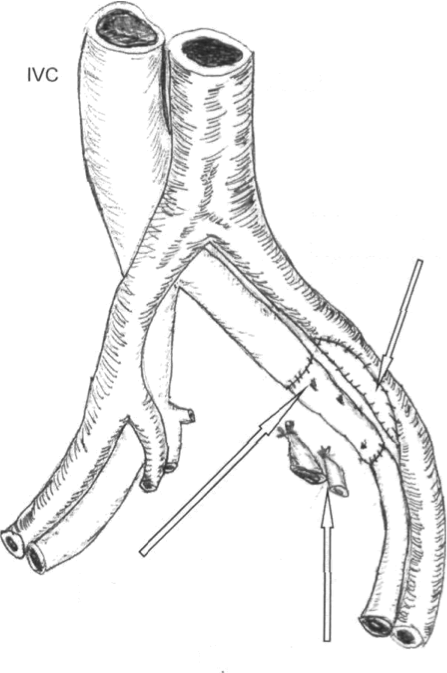
FIG. 3. Bypass of the left external iliac to common iliac vein with an interposition graft using (he contralaieral superficial femoral popliteal vein with vein patch repair of the artery
THE AMERICAN SURGEON
January 2006Vol. 72
They perfomied simultaneous iliac vein and an artery bypass with 1O-mm externally supported polytelrafluoro ethylene (PTFE) for a large reiropcritoneal fibromatosis. The venous bypass was supported by an arteriovenous (AV) fistula graft, which was taken down after 8 weeks. This is a reasonable approach when the margins are limited to retroperitoneal structures not involving bowel. Prosthetic grafts also have been used for inferior vena cava reconstruction in urologic malignancies.4 Autogenous conduit is more resistant against infection and is also less thrombogenic than synthetic graft. Limitations with the greater saphenous veins are size mismatch and availability. Internal jugular vein can be an excellent large-caliber autogenous graft when operating in a contaminated field. It has been described for reconstruction of femoral veins.5 However, a limitation for using an internal jugular vein is graft length. Also, it may be unusable due to multiple previous intravenous line placements. Furthermore, it can be quite cumbersotne to work at two different surgical fields. Superficial femoral vein has shown excellent patency and resistance to infection in arterial and central venous reconstructions.6 Having an autogenous in-line conduit is advantageous when subsequent catheter access to the inferior vena cava (IVC) tnay be required. The surgeon has the ability to choose the appropriate length and work within the same surgical field. Finally, a surgical resection with a potential to obtain negative margins can be achieved. This case illustrates the technical feasibility of simultaneous
arterial and venous reconstruction after an en bloc resection for what could have been "unresectable" recurrent cancer, lo the best of our knowledge, the use of femoral vein has not been described as a conduit in pelvic exenterative surgery requiring venous reconstruction. The patient was placed on warfarin for 6 months after discharge. He was also placed in compression stockings for 6 months. Follow-up duplex after 1 year did not reveal any obstruction in the iliac system with the venous graft still patent. There were no symptoms of venous morbidity or deep vein thrombosis (DVT) on either side.
REFERENCES
1. Nccl HB. Ketc-ham AS. Hammond WG, Joseph Wt.. Vascular comptications fallowing cancer surgery of the pelvis and groin. Cancer 1970:26:669-79.
2. Crawford ES, DebaLey Mf. Wide excision including in- volved aorta and vena cava replacement with aortic homograft for retroperitoneal malignant tumor. Cancer 1956:9:1085—91..
3. Piquet P. Delpero JR. Pol B. et ai. Vascular reconstruction afler extended resection of retroperitoneal fibromatosis. Surgery 1990:107:346-9.
4. Caldareili G, Minervini A, Guerra M. et ah Prosthetic replacement of the inferior vena cava and the iliofemoral vein for. urologically related malignancies. Br J Urol Int 2002;90:368-74.
5. Hill S. Thomas JM, Nott DM. Reconstruction of the iliofemoral venous circulation using internal jugitlai" vein autograft Ann R Coll Surg Engl 1997;79:460-i.
6. Hagino RT. Bcngston TD. Fosdick DA. et al. Venous reconstructions using the superficial femoral-popliteal vein. J Vase Surg 1997;26:829-37.
3/10/2021
AHSAN T. A£I, M.D.,* G. PATRICK CLA GETT, M.O.,I MICHAEL J. E DWAIt DS, M.D.*
Published January 2006
AHSAN T. A£I, M.D.,* G. PATRICK CLA GETT, M.O.,I MICHAEL J. E DWAIt DS, M.D.*
Complex Venous and Arterial Reconstruction with Deep Vein After Pelvic Exenterative Surgery
Summary
A patient with recurrent rectal cancer had the cancerous mass at the middle of the an iliac vein & an iliac artery. To remove it, vascular surgery & reconstruction was required.
After the tumour was removed, arterial & venous reconstruction was done using bypass & prosthetic grafts. This proved that simultaneous arterial & venous reconstruction is possible.