-
Endovascular Approach to Chronic Mesenteric Ischemia
AHSAN T. ALI and MATTHEW R. ABATE
Presentation
A 62-year-old man underwent an aortofemoral bypass graft (AFBG) for occlusive disease. In the immediate post-op period, he suffered mesenteric ischemia and underwent bowel resection (sigmoid and small bowel). Postoperatively, he developed aortic graft infection and nonhealing groin wounds in the setting of severe malnutrition and failure to thrive. Subsequent workup included computed tomography scan (CTA) demonstrating a stenosis of the superior mesenteric artery (SMA) and an occluded celiac artery.There was uid around the graft indicating pan graft infection. Meanwhile, the patient had lost almost 35 pounds, and his prealbumin was 8.1 and albumin was 1.2.
Differential Diagnosis
There is usually little ambiguity about the diagnosis by the time the patient arrives in vascular clinic. Most patients have already undergone a cholecystectomy along with esophagogastroduodenoscopy (EGD) and colonoscopy, along with further imaging studies such as a CTA.
The hallmark of chronic mesenteric ischemia (CMI) is weight loss and postprandial pain. In certain clinical scenarios, the diagnosis can be in question if there is no weight loss. Occult malignancy can be associated with weight loss and“aversion from food”due to nausea. Thus, in patients with a history of smoking and unexplained weight loss, occult malignancy has to be ruled out before embarking on any mesenteric revascularization therapy. Other differential diagnoses to consider include nonoc- clusive mesenteric ischemia at watershed areas, median arcuate ligament syndrome, and aortic dissection.
Workup
In addition to history and physical examination, nutritional parameters and contrast imaging are essential in diagnosis and preoperative planning. CTA is most commonly uti- lized and will also demonstrate collateral pathways such as the arc of Riolan and marginal artery of Drummond. Other subtle ndings are calci cation of the origin of the SMA.
Case Continued
The patient had weight loss and postprandial pain. The preoperative CTA demonstrated severe stenosis of the SMA and occlusion of the celiac artery. The CTA also showed the presence of collaterals between the SMA and the inferior mesenteric artery; mainly the arc of Riolan and marginal artery of Drummond. The patient was scheduled for an arteriogram via the left brachial approach as an ini- tial attempt to revascularize the SMA or the celiac artery.
Surgical Approach
Endovascular revascularization of the mesenteric ves- sels is indicated in acute or chronic clinical settings. A bypass to the celiac and/or the SMA from a supraceliac approach has the highest patency but comes with sig- ni cant morbidity and mortality. However, if the patient is at a high risk, then an endovascular approach can be initially utilized as a bridge to an open and more dura- ble procedure. The current trend is an endovascular approach rst. Open mesenteric revascularizations are being performed less, and most vascular graduates have been exposed to only a handful of cases during their training. Hence, this trend may very well have to do with the comfort level of the vascular surgeon. However, the authors believe, an initial endovascular approach for CMI serves as a bridge to open surgical therapy espe- cially if the patient is severely malnourished or very high medical risk.
For endovascular treatment of CMI, several things have to be considered: brachial versus femoral approach, type of catheter to engage the lumen, balloon expandable stent versus self-expanding, covered versus bare metal stent, and monorail versus coaxial systems.
Contraindications to Endovascular Approach
There are no absolute contraindications. Occlusions of the SMA with heavy calci cations can be a relative contraindi- cation, especially if the occlusion is up to the middle colic artery.
Celiac vs. SMA or Both
The main objective is to treat the SMA. Celiac artery stenting can be attempted if SMA angioplasty is not possible or can not be done. In a comparative analysis of celiac versus SMA angioplasty and stenting, Ahanchi
et al. found the primary patency of SMA interventions to be signi cantly higher bringing to question the clinical utility of celiac artery angioplasty and stenting. Unlike an open bypass, revascularization of both celiac and SMA is not the norm when attempting endovascu- lar approach.
Angioplasty Versus Stenting
Stenting is recommended as the patency of angioplasty alone is dismal.
Brachial Versus Femoral
A femoral approach is preferred by some because it accommodates a larger sheath and a closure device can be used. For this particular approach, a curved catheter such as a Visceral Select (Cook Medical, Bloomington, IN) with a“Shepherd hook”is used with a hydrophilic wire. A Glide Cobra (Terumo Medical Corporation, Tokyo, Japan) can be used as well. However, a ush occlusion of the SMA usually precludes the femoral approach. The left brachial artery provides a straighter approach but has a higher complication rate. With access via the left bra- chial artery, the catheter does not need to be reversed;
a Vert or MPA 125 are popular choices (Cook Medical, Bloomington, IN). This approach can be performed with a cut down in high-risk patients (women, small caliber arteries). Lastly, it also depends on skill set and comfort level of the surgeon. The brachial approach clearly has advantages of torquability and pushability to facilitate crossing occlusions.
Balloon-expandable Versus Self-expanding
Most interventionalists prefer a balloon-expandable stent for accurate placement. However, if an abdomi- nal procedure is planned in the future, a self-expanding stent can be used. It will keep its form and withstand retractor pressure during a subsequent open procedure, whereas the balloon-expandable stent may get crushed. Self-expanding nitinol stents are not as precise. Avoid the usage of more than one stent.
Covered Versus Bare Metal
With covered stents there are four options: Gore ViaBahn (Gore Medical, Flagstaff, AZ), Bard Fluency (Bard, Tempe, AZ), Wall Graft (Boston Scienti c, Natick, MA), and iCast (Atrium, Hudson, NH). The rst three require a large
TABLE 1. Key Technical Steps and Potential Pitfalls
Key Technical Steps
1. Approach via the left brachial artery. The authors recommend a cut down if the patient is at high risk for brachial complica- tions (elderly, women, small caliber arteries). A femoral approach can be used, if the angle of the SMA is not very acute.
2. Place a 6-French 90-cm sheath if approaching via the brachial artery in the descending thoracic aorta at the level of the celiac artery (a 70-cm sheath is not long enough in most instances). Imaging can be obtained from a femoral sheath simultaneously through a separate catheter.
3. The image intensi er is placed at 80–90 degrees for a lateral view and initial angiogram obtained to identify the SMA and the celiac artery. The patients upper extremities have to be out of the way (above the head) for better imaging.
4. A slightly angled, moderately stiff catheter (e.g., MPA 125) is used with a hydrophilic stiff wire such as a Road Runner or Stiff Hydrophilic Glide (Cook Medical, Bloomington, IN) for crossing an occlusion. If there is a high-grade stenosis, a more pliable wire is preferred.
5. Once the wire has crossed the lesion, exchange it with a 0.35 or 0.18 working wire. Have adequate purchase of the exchange catheter into the target artery as it may get kicked out when introducing a stiffer wire, especially from the femoral approach.
6. Advance the sheath to cross the lesion, especially an occlusion.
7. Balloon angioplasty with a 20- to 40-mm length balloon can be used to assess the extent of area to be treated and visualize the waist seen during insuf ation.
8. Once the stent is in the desired location, withdraw the sheath.
9. Deploy the stent hanging out 3–5 mm into the aorta as it is easy to miss disease at the origin. The angle of the SMA has to be factored in to have adequate coverage.
Potential Pitfalls
• The stent can sheer off the delivery catheter when going through a long heavily diseased segment. Hence, the sheath or guiding catheter should cross the lesion rst if a balloon-expandable stent is used. Similarly, predilating with a balloon can make crossing the lesion with a stent less risky. This can be dif cult if 0.18 or 0.14 wires are used, as they may not be able to provide enough support. Thus, the sheath has to cross the lesion on a 0.35 system.
• Plan on placing a single stent. Magnify the image during deployment for precision, as it can be dif cult to visualize the extent of the diseased segment and the origin of the vessel.
• The lesion may require preangioplasty for the mounted stent to go through. During this, very judicious wire control cannot be over emphasized since there is not much purchase in the SMA and wire access can easily be lost. In addition, the location of the wire must be identi ed so it is not in one of the smaller SMA branches, which can lead to a perforation. Wire movement is inevitable during the procedure, and utmost caution has to be used to keep ensuring the position of the wire.
• Dissection of the SMA is a dreaded complication. It can be avoided by minimizing wire and sheath movement with catheter exchanges. Also, avoid advancing the sheath unprotected without a dilator.
380 Clinical Scenarios in Vascular Surgery
caliber sheath (7 French or greater) and usually cannot be very precisely placed via the femoral approach. Hence, a cut down of the brachial artery may be necessary. The author prefers a balloon-expandable bare metal or cov- ered (iCast, Atrium, Hudson, NH) stent. These can be deployed using a 6-French sheath. The longer the stent, the more dif cult it is to deploy accurately. Anything lon- ger than 40 mm is usually not needed.
Special Intraoperative Considerations
Abandon the procedure if:
1. The lesion is heavily calci ed and there is a long seg- ment occlusion in a small caliber vessel.
2.Flush occlusion of the SMA precludes femoral approach.Case Conclusion
The cross table oblique arteriogram con rmed a high-grade proximal SMA stenosis and occluded celiac artery. A balloon-expandable bare metal stent (8 × 20 mm) was successfully placed in the SMA (Fig. 1).
He was then placed on nutritional supplements for the next 2 weeks.The patient gained weight while he was on supplemental nutrition and IV antibiotics. He then underwent replacement of the infected graft with femoral vein and has continued to do well postoperatively.

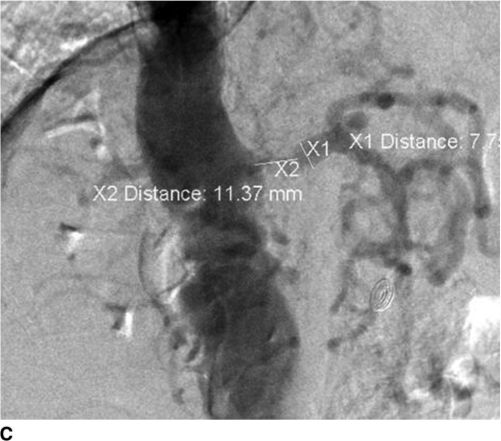


FIGURE 1 • A: Arteriogram from a steep oblique to show the origin of the SMA and high grade stenosis as indicated by arrow. B: After angiogram, measurements are made to size the PTA/stent with a 10-mm arterial size and 1.1-cm length. C: A con rmatory image with in ated balloon. D: A post-PTA/ stenting arteriogram shows brisk ow without stenosis.
77 • Endovascular Approach to Chronic Mesenteric Ischemia 381
TAKE HOME POINTS
• Endovascular approach is usually a“bridge”to an open procedure in a severely malnourished patient where a combined mesenteric bypass and a major open procedure is a prohibitive risk.
• Use long sheaths and long catheters from the out- set of the procedure. A stent will be needed for all ostial lesions. Avoid stenting long segments that extend to the middle colic artery and are heavily calci ed.
• Balloon-expandable covered stents are available in 6 mm diameter through a 6-French sheath system. A brachial approach is preferred for a more anatomi- cally aligned stent.
SUGGESTED READINGS
Ahanchi SS, Stout CL, Dahl TJ, et al. Comparative analysis of celiac vs mesenteric artery outcomes after angioplasty and stenting. J Vasc Surg. 2013;57(4):1062-1066.
Brown DJ, Schermerhorn ML, Powell RJ, et al. Mesenteric stenting for chronic mesenteric ischemia. J Vasc Surg. 2005;42(2):268-274.
Eidt JF, Mills J, Rhodes RS, et al. Comparison of surgical opera- tive experience of trainees and practicing vascular surgeons: a report from the Vascular Surgery Board of the American Board of Surgery. J Vasc Surg. 2011;53(4):1130-1140.
Fioole B, van de Rest HJ, Meijer JR, et al. Percutaneous trans- luminal angioplasty and stenting as rst-choice treatment in patients with chronic mesenteric ischemia. J Vasc Surg. 2010;51(2):386-391.
Kalapatapu VR, Murray BW, Palm-Cruz K, et al. De nitive test to diagnose median arcuate ligament syndrome: injectionof vasodilator during angiography. Vasc Endovascular Surg. 2009;43(1):46-50.
CLINICAL SCENARIO CASE QUESTIONS
1. A 77-year-old woman presents with mild abdominal pain 3 weeks after colon resection for a left colon mass. She has a normal lactate but elevated WBC to 16K. Postoperatively, she has not been eating well and lost weight. After evaluation, mesenteric ischemia is sus- pected. She has an occlusion of the SMA 1.5 cm distal to the origin all the way to the middle colic on CTA. The celiac artery has a high-grade stenosis. What is the most appropriate approach:
a. Systemic heparin and open embolectomy of the SMA
b. Systemic heparin with systemic vasodilator
c. Systemic TPA
d. Angiogram via brachial approach and stent the celiac artery rst
e. Angiogram via the brachial artery approach and stent the SMA rst past the middle colic
2. Decreasing the risk of mesenteric arterial dissection with an endovascular approach is best accomplished by:
a. Using intravascular ultrasound
b. Always approaching the artery ori ce via a groin approach
c. Preprocedural clopidogrel loading
d. Care with advancing the catheter or sheath only after good wire access
e. Using self-expanding stents only

3/10/2021
AHSAN T. ALI and MATTHEW R. ABATE
Published 22 January 2015
AHSAN T. ALI and MATTHEW R. ABATE
Endovascular Approach to Chronic Mesenteric Ischemia
Summary
Chronic Mesenteric Ischemia can be fatal in a severely malnourished patient. This is why an endovascular approach is the best option. It acts as a bridge to an open and more durable procedure.